My name is Dr. Haroun Gajraj. I’m a vein specialist and I trained as a vascular surgeon in London and did most of my surgical training in London. I took up an appointment in Somerset as an NHS consultant -17 years ago now and treated the whole range of vascular problems : arteries veins and other problems; but about five years ago I left the NHS to concentrate exclusively on the treatment of veins and that’s all I’ve been doing now for five years. I’ve given up all my arterial work and I just deal with vein problems.
Well what are varicose veins? Well you don’t need to be medically trained, you don’t need to be a doctor to look at your leg or somebody else’s leg and know that there’s something wrong with the veins. So for example this person has a cluster of spider veins at the back of the leg with varicose lumpy veins to the side; and medically they are abnormally large . They’re wider and bigger than they should be they’re of obviously twisty and turny and they have a condition in them called reflux. Veins should be carrying blood up the leg back from the foot to the heart. If the little folds in the lining are not meeting properly and gravity is pulling blood down in the wrong direction then we give this the term vein reflux; and the underlying problem with these thread veins and these spider veins is that the direction of flow is wrong; the valves are not working properly; and blood is coming down in the wrong direction; that’s the medical underlying problem.
What causes varicose veins? Well, top of the list is heredity. Unfortunately you can pick your friends but you can’t pick your parents and most cases of vein problems are inherited or have a genetic basis. It’s been estimated that if both your parents have a vein problem then you unfortunately have an 80% chance of developing a vein problem yourself. It’s not inevitable but it’s a high risk if you have a strong family history. Other things on this list don’t actually cause varicose veins but they contribute . So, if you’ve inherited a weakness of your veins and you have an underlying problem often veins will appear for the first time during pregnancy because of the added strain on the vein circulation. It doesn’t actually cause it but it’s another risk factor which declares itself if you have an underlying problem; and all these other things contribute. Having said that, we know lots of people don’t we who have had lots of children,who are probably or possibly overweight and don’t have a particularly healthy lifestyle- not a blemish on their legs. It doesn’t seem fair does it really but equally there are many young men who are quite athletic and very fit that obviously they’ve never had any children themselves and they’ve got dreadful varicose veins. So it does appear that heredity is the main risk factor.
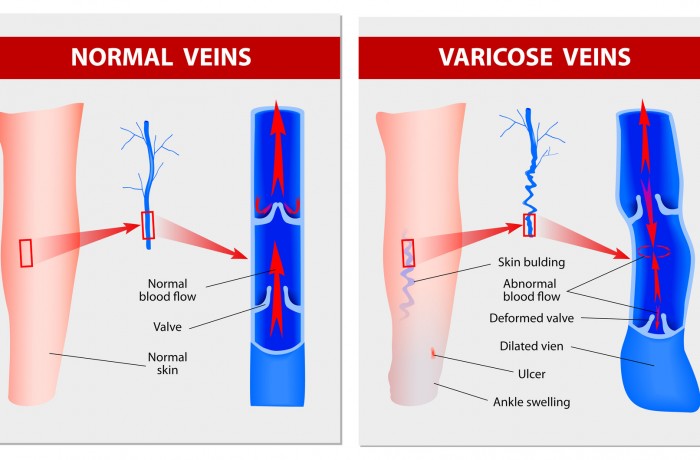
What causes thread veins? Well I’ve already mentioned that reflux is the underlying problem, so it’s not a surprise really is it that top of the list is heredity. Again many people have not a blemish on their leg because they’ve inherited good veins from their parents. Others unfortunately haven’t had any children, not overweight, very healthy and they are covered in in spider veins and thread veins. The underlying problem is a weakness of the veins and it’s a problem called reflux. So heredity tops the list. All these others are contributing or risk factors; they don’t actually cause them. However I would say that reflux which also causes varicose veins. Varicose veins are often associated with thread veins. In fact when I see people with thread one of the important things is that you check very carefully for underlying reflux, so that the problem is treated correctly. Are they simply cosmetic? Well a something I get asked a lot is “I’ve been to my doctor with my veins and he tells me that the treatment is not available on the NHS”; and often that person is told that they’re “simply cosmetic”. Well they’re not simply cosmetic. As you can see from this slide: A healthy vein is nice and straight and it’s got strong folds, strong valves in the lining, that meet properly keeping blood directed upwards from the leg back to the heart. On the right we have a varicose vein: it’s wider than it should be it’s torturous: it’s “wiggly”; and the valves these little folds are weak and floppy and they’re allowing blood down in the wrong direction. So varicose veins are unhealthy veins with faulty valves and this condition called reflux. So it’s not simply a cosmetic issue as you can see, in this slide, we’ve got a leg where we’ve got a superficial vein that’s a vein underneath the skin that is refluxing and faulty and the blood is coming down in the wrong direction from the top of the thigh down into these lumpy varicose veins and further down into these little spidery veins. So the underlying problem is reflux; it’s not simply a cosmetic issue. It’s a shorthand way of saying the majority of people don’t get major problems but to dismiss them as simply being cosmetic is not correct.
This is a lady I saw a few years ago and she too was denied NHS treatment initially. She had quite bad reflux in the veins in her thigh feeding into varicose veins in her calf which were causing quite a lot of swelling of her leg and they were causing quite a lot of thread veins and spider veins around the ankle. And also after a little while were causing a condition called varicose eczema which I’ll come on to in a moment. In her case they weren’t simply cosmetic. She actually had to argue her case quite strongly and at that time had to appeal to the Primary Care Trust, the PCT. Eventually she was granted NHS treatment but her operation was canceled three times; twice on the day of her operation. She’d been all more prepared, got ready and in frustration she decided that she would have a veins treated privately. She was concerned quite rightly about the possibility of ulcers. So what problems can arise? One of the questions I get asked again quite a lot is- “I’ve got bad varicose veins will I get a leg ulcer? I’m worried about leg ulcers”. Well in fact the majority of people with even quite severe varicose veins do not come to any harm and I think this is the main reason why the NHS doesn’t treat veins. They do however cause a lot of ache, a lot of itch swelling. These symptoms do tend to be worse in hot weather; they tend to be worse at the end of the day; and they’re also very unsightly.
I think it’s sometimes difficult for us men to understand how much distress it they caused to women particularly and increasingly men. It interferes with what you can wear, what sort of holidays you can take, what sort of social activities you might be involved in. I came across a lady not so long ago who wouldn’t take her children swimming because she felt so embarrassed about the sight of her legs. And the distress that some of these unsightly veins cause can be quite severe. I say “even thread veins”, we now know that thread veins and spider veins are associated with this condition called reflux so it’s not surprising that even thread veins cause symptoms or are associated with symptoms. Until we knew a little bit more about the condition we didn’t really as doctors believe people who say well my “my thread veins hurt and they burn and they itch”; but they do and we now know that if you treat thread veins properly, the majority of people get relief of their symptoms as well. So, as I say, a frequent question is I’ve got bad varicose veins will I get a problem? Well the majority don’t but if you do get medical problems they come under one of these four headings. As I say the majority will not.
The first one I’d like to talk about is phlebitis. A frequent question is “I’ve got phlebitis, what is it and will it cause me any harm. Another condition is varicose eczema, a condition of the skin caused by reflux; and these other conditions deep vein thrombosis bleeding and ulcers. Let’s talk about those very briefly in turn. Now phlebitis is often a misused term, both by the public and by doctors. The strict medical definition of phlebitis is an inflammation in the vein – that’s all it means really. Doctors add the word “-itis” on the end of the word to indicate inflammation. I think “phleb” is from the Greek or Latin word that means vein and “itis” means inflammation. So it’s an inflammation of the vein. It appears clinically, that is on the surface, as a hard, tender lump underneath the skin. So it’s quite superficial: phlebitis involves the superficial veins. It’s superficial and it has all the features of inflammation.
So if you’ve ever had inflammation elsewhere you’ll know that it’s red, warm, tender; and its quite a severe condition: these people often can’t go to work it’s that painful. It used to be thought to be quite a trivial condition . So if you went to see your doctor he’d say “Oh that’s just a bit of phlebitis, take some painkillers and go away”. We now know however that to diagnose phlebitis correctly you should have an ultrasound scan. People who are diagnosed as having phlebitis are often misdiagnosed; and when you look with an ultrasound scan there’s another condition. So having an ultrasound, firstly confirms that it is phlebitis, because you can actually look at the superficial vein and the appearance on ultrasound is quite characteristic of the condition; and you can make sure there’s nothing else amiss because we now know that phlebitis is frequently associated with deep vein thrombosis. The clot that occurs inside these veins can extend further and into the deep veins and that can be quite a significant problem, quite a severe condition. Last week, I saw a patient in Bristol who had been treated by his doctor for phlebitis and in fact he had a deep vein thrombosis all along. So the diagnosis was wrong: it would have been established with an ultrasound scan; and he had there quite a significant deep vein thrombosis that put him at risk. So phlebitis is not a trivial condition; it should now have an ultrasound scan. That’s the recommendation of two very influential bodies, one in the United Kingdom and one in America and that recommendation came out last year – that all people with phlebitis should have an Ultrasound Scan. I don’t know if anyone reading this has had phlebitis and whether they had an ultrasound scan but I think now if you have been told or you suspect you’ve got phlebitis you should have an ultrasound scan.
Varicose eczema: this is a condition that affects the skin usually just above the ankle. Now this is a term that is misleading. You might think well “Varicose Eczema” – it’s a skin problem – and indeed I see many people who are treated with creams, often steroid creams. These conditions are very itchy – they can drive you mad -and they can keep you awake and they can cause a lot of distress and there’s no doubt that there is inflammation of the skin and there’s no doubt that if you put steroid cream on you will feel better: the itching will go; your leg will feel better and it’ll give you some relief. Varicose eczema is not principally a skin condition: It’s due to this problem called reflux and what this indicates is that the skin is being damaged by this faulty vein circulation. It looks like “eczema” but it actually indicates that there’s damage to the skin and that that skin is vulnerable and at risk of ulceration. So this condition is often the precursor of a leg ulcer: not tomorrow, not the day after; it takes takes time but the skin is vulnerable and at risk and this should be treated to prevent an ulcer. It’s not a skin condition it shouldn’t really be treated with steroids. In fact steroids if you put them on long term, they actually thin the skin and they make the skin more vulnerable, more liable to ulceration. So varicose eczema should be treated by a vein specialist or a vascular surgeon: not a dermatologist and not with skin creams.
Deep vein thrombosis: well this is the fear of most people. In fact it’s not very common as a complication of veins. It’s only recently that we are confident now to be able to say that varicose veins are a risk factor for deep vein thrombosis. There’s now good evidence in the medical literature to support that. It doesn’t mean you’re going to get one inevitably, but if you have an additional risk factor, varicose veins will contribute. So for example, if you were to go into hospital and have major surgery, say a hip replacement or a major operation for bowel cancer and you had bad varicose veins, it would slightly increase your risk of a deep vein thrombosis. If you were to go on a long-haul flight with bad varicose veins, it would add to your risk. It doesn’t cause it, but it is a risk factor . And anyone under those circumstances coming out of hospital after surgery stepping off a plane after a long-haul flight who has one leg more swollen than the other, it should ring alarm bells- “have I got a deep vein thrombosis?” And again, the only way to diagnose deep vein thrombosis accurately, or to exclude it, to say “no you don’t have a deep vein thrombosis” is to get an ultrasound scan. Now the next slide is a little bit scary I’m sorry I keep meaning after these presentations to take it out and put a less scary slide in it is a little bit scary if you’re squeamish look away. Having said that most people wake up at this stage and it’s the slide they all want to see. This is a leg ulcer this is the dreaded complication of varicose veins and reflux. Once they develop – this is quite a severe one – once they develop, they’re very difficult to heal, they’re very difficult to eradicate. Even when you do get them healed, they heal with a lot of scar tissue; the area is quite vulnerable and it’s never quite normal. So it’s always a little bit more vulnerable to knocks and injuries. So leg ulcers once they’re established do tend to recur, even withthe best available treatment, because of the vulnerability of the scar tissue. So avoid leg ulcers if you can. I’m sure you don’t nobody wants a leg ulcer but if you’ve got varicose eczema and you’ve got any complications from your veins, we know that early treatment will give better results and will reduce the risks of complications.
So as I mentioned many people go and see their doctor they say I’ve got vein problems but the NHS doesn’t treat them. Why is this ? Well the NHS doesn’t see veins as a priority and the majority of people even with quite severe vein problems don’t get a major complication. The NHS is strapped for money. I think we have to accept that and there are other more pressing requirements. There’s no national target for veins; there’s no 2-week wait for veins and there’s no targets as there are as you’d expect for an ambulance arriving. We all expect if we’re injured that an ambulance will arrive within a certain time . We all expect that it will take us to a well-equipped hospital with an operating theatre if we need urgent surgery and we all expect that if we suffer a heart attack we’re taken to coronary care and we looked after. This all costs money and obviously the NHS has limited resources. I don’t want to get too political but you can imagine that if the majority of people don’t get a major problem from their veins the NHS can’t treat any everybody. It has to ration treatment. the National Institute for Care and Health Excellence -NICE- last year 2012- no 2013 – earlier this year only in the summer of this year made several recommendations about the treatment of veins and it said specifically that anyone who’s got symptoms from their veins should be referred to a vascular surgeon. However we know and I know that currently people even with varicose eczema are finding it difficult to get NHS treatment. So although NICE believes that people should have advice the reality here in this area is that people are finding it difficult to get access to treatment. Other reasons. Thread veins are often regarded as cosmetic when we now know that the majority of people even with red veins have reflux. Varicose veins are not a priority as I’ve mentioned. There are other more pressing problems for the limited resources of the NHS. I was going to say it’s rationed by strict criteria. They seem to be getting stricter and stricter and access seems to be getting poorer and poorer as time goes by and I see people who have had bad phlebitis or who’ve had varicose eczema and who can’t get treatment – very difficult. And obviously your doctor needs to keep up-to-date with all sorts of new developments in diabetes and blood pressure and child care and dementia ,he finds it very difficult to keep up to date with all the latest treatments on veins. Not surprisingly, your your GP may not be able to refer you to the local hospital for veins so at the end of a busy surgery is hardly going to read up, spend hours, reading on the latest developments on veins. What treatments are available?
Well we categorise them into one of these four sections:there’s graduated compression hosiery – that’s medical stockings; we’ve got the surgical stripping operations which some of you in the audience might have had;there are injection treatments – sclerotherapy which I’ll cover in a moment and then there are some new treatments which are done through tiny little punctures on the skin- we call them keyhole type procedures they either involve heat energy or they involve superglue which is one of the latest developments which I’m going to cover very shortly. Now whenever anybody thinks of medical graduated compression hosiery I think of Nora Batty and it is true that a lot of medical stockings are those beige or brown thick wrinkly things that won’t stay up, difficult to get on. This is just us to show you that good quality Modern Medical Compression hosiery doesn’t have to be like that, it doesn’t have to be stigmatising. Now it’d be nice if you put a pair of stockings on like that and your legs instantly look glamorous, but the important thing to take away is that it isn’t stigmatising; they do look nice they are comfortable and your legs tend to fee lbetter when you when you wear them. Now they’re not support tights they’re very different. They’re graduated which means that they’re firmer at the ankle and they give a certain amount of squeeze measured in so-called millimeters of mercury. That’s the same measurement that we use to measure blood pressure. So it gives a certain amount of squeeze at the ankle and then progressively less as yougo up the leg and it works with the vein circulation. Now some of you may be familiar with Kalipos or popsicles those are ice lollies which you squeeze at the bottom and they come out of the packet. Yes? Some nods there. Well if you if you squeeze firmly at the bottom up comes the ice lolly. If you squeeze the same all the way up and down even if you squeeze quite hard the ice lolly doesn’t move. So it has to be squeezed at the bottom firmer than the rest and up comes the lolly. In the same way, if you squeeze the ankle slightly more than the rest of the leg,in that fashion, it works with the vein circulation encouraging the blood flow back up the leg. Is medical grade compression a cure for varicose veins? Well, clearly not. Whilst you’ve got the medical sock on or the medical stocking on it resists the reflux, it corrects the reflux but when you take the stocking off, obviously the blood comes down in the wrong direction and the varicose veins or the problems recur. But whilst you’re wearing a medical grade compression stocking, your legs will feel better, so most of the symptoms will get much better whilst you’re wearing them, if not be abolished completely. There is quite a bit of evidence that it will reduce the progression of the vein problem and reduce the risks of complications. We know that medical grade compression stockings reduce the risks of a deep vein thrombosis in certain situations . So for example on long-haul flights, going into hospital, they reduce that risk of deep vein thrombosis. And if you’re unfortunate enough to have had a deep vein thrombosis then I would suggest that you should wear good quality medical grade compression hosiery. Again, very recently I saw a man who’d had a very big deep vein thrombosis five years ago, unfortunately once you’ve had a deep vein thrombosis it does damage those delicate valves in the deep veins. Deep veins cannot be treated by surgery, superficial veins can but deep veins can’t. He had damaged his deep veins with his deep vein thrombosis and after five years he had developed quite a nasty leg ulcer. Unfortunately he hadn’t been advised about wearing medical grade compression hosiery which I think would have prevented him from developing a deep vein thrombosis. This is something unfortunately we see quite a lot of in our clinic.
Surgical stripping. Well some of you might have had this operation. Until recently it was the commonest way of treating veins. I think it is still performed in the NHS , though NICE that body I told you that says everyone who has symptoms should be referred, NICE has also said that surgical stripping is out now. Surgical stripping which was invented about 200 years ago, in 2013 NICE said that’s the end of surgical stripping. It should be third choice after endovenous thermal treatments which I’ll talk about in a moment and injection treatments -Sclerotherapy- but what it involves is going into hospital,having a general anaesthetic and then a cut in the groin here and then this refluxing vein in the thigh has a piece of surgical wire put down it. The surgical wire often travels down to the ankle or into the calf another surgical cut is made in the calf to find that wire and then the surgical wire has pulled out. A lot of you are cringing now the sight of that or the description oft that. Yes, it wasn’t something that most people wanted to have done . Very few people wanted to go in hospital and have painful cut in the groin and their veinspulled out. It did have a reputation for being quite painful. A lot of people,particularly if they had both legs treated, couldn’t go to work for six to eight weeks – it was that painful. They couldn’t drive for ten days. I think two or three weeks off work one leg if you’re very motivated if you have both legs treated you’re going to need a month or two. And after being subjected to all of that, the real problem with surgical stripping is that it had what’s called a very high recurrence rate, which meant that the veins come back. Having been through all of that, few years later the veins come back.We now know that surgical stripping – when you cut a vein and tie it off and pull a portion out – the two raw ends of the vein want to regrow and rejoin. We didn’t believe, as surgeons, that this could happen. If you cut a vein here at the top of the thigh and pulled it out to the calf or below the knee that that vein could regrow, but because we now have the widespread use of ultrasound, we can follow patients at intervals and we can see the veins re growing and again being doctors we like to give a fancy name to this we call it neovascularization, which just means that new veins have regrown. So third choice now according to NICE. The dominance of surgical stripping is over hopefully in the next year or two we should see surgical stripping coming off the scene – altogether and this slide will probably have to be taken out of my presentation. But we’ll still see a lot of people who’ve had surgical stripping5, 10, 15 years ago, who will be coming back with recurrent veins because, as I say, it does tend to be associated with recurrence.
Sclerotherapy: sclerotherapyis an injection treatment we can now identify faulty veins with ultrasound and guiding the needle into the vein we can inject a prescription medicine called asclerosant into these veins. I’m sorry. So veins that were previously only treatable by stripping, can be injected with a prescription medicine. And it works by removing the lining of the vein- it does that within a few seconds of the injection – and that doesn’t hurt surprisingly. And then the vein responds over the course of time by shrinking and closing. So this vein here in the thigh that would be surgically stripped in days of old, we can now identify with ultrasound and inject with a sclerosant. Now the sclerosant that we use can be turned into foam; some of you may have heard of foam sclerotherapy. We can take the prescription medicine that comes as a liquid in the ampule and because it is biochemically a detergent, we can mix it with air in a certain way to turn it into foam. If you take washing-up liquidand splish and splash it makes bubbles and foam. ell we can do this in a more controlled way with the sclerosant and turn it into foam and we can inject that into this refluxing vein. Now it’s not like cavity wall insulation, it doesn’t stay in the vein forever. What it does is it will displace the blood push the blood out of the way, sit in the vein do its job and then after a few minutes it will disperse back into a liquid and be eliminated from the body. And foam sclerotherapy has revolutionized treatment of refluxing veins. It was invented in 1995 and there have been number of medical studies now showing that it’s just as effective as surgical stripping; and that’s why it has replaced surgical stripping it’s now in number 2 slot according to NICE. Surgical stripping is number3 slot. The advantages are that it doesn’t require a general anaesthetic, you have very minimal time off work, it’s a walk-in walk-out procedure and it has been described as a lunchtime procedure. There are no cuts or scars and you can get back to normal activities pretty much straightaway, So a lot of advantages compared with surgical stripping.
The other treatments we have are so-called endovenous thermal treatments. Now this is a way of saying that the vein can be treated from the inside using heat energy; and here you can see a little schematic which shows that the refluxing vein has a very small catheter inserted into it under ultrasound guidance. That catheter is then inserted or guided right up to the top of the leg – you don’t feel that surprisingly -you may feel a little tickle under the skin of the thigh but you don’t tend to feel that. And once it’s in position very carefully, again confirmed by ultrasound, you can numb this vein up with local anaesthetic and you can heat the vein to a temperature at which it is closed. It is cauterised, sterilised and devitalised; and as the catheter is withdrawn that vein is closed all the way down . So that when that person gets out of bed first thing in the morning and stands up, blood is no longer refluxing down this vein and is no longer filling the varicose veins and thread veins further down. As you can see in this little schematic, the varicose veins shrink and return to more normal size now .
One of the questions I get asked quite a lot is “I’ve got bad varicose veins, if I have my veins treated or removed what happens to the blood?” Well that’s a very good question. The important thing to realise is that we have two sets of veins in our leg: a deep set which lie deep within the muscle; and a superficial set which lie just underneath the skin. It’s the deep set that carry most of the blood up your leg. The veins under the skin don’t actually carry very much blood at all. And even more important than that is that we only treat unhealthy veins . We identify the refluxing veins with ultrasound and we’re only treating those. So imagine a situation in which your deep veins are pumping the blood up your leg and the superficial veins are letting blood down your leg. That would be a little bit like carrying water from one place to another in a bucket with a hole in it. You need to make more trips. If we plug the hole, you need to take fewer trips. Well by dealing with refluxing veins in this way, the deep veins can pump the blood up the leg and there’s less spillage down the leg. So actually your deep veins could do their job more efficiently; and that’s why by treating reflux and varicose veins your leg will feel better because we’ve taken the pressure and the work off the deep veins .
The good thing about endovenous thermal treatments is again they’re local anaesthetic; they’re walk-in walk-out; there’s no painful cuts and scars; and there’s minimal time off; there’s rapid results. And the really good thing is that they have the lowest recurrence rate. So the risk of that vein ever recovering is very very low. In fact I haven’t seen a vein recover from anendovenous thermal treatment done properly in 12 years. So it’s a very good treatment. there are various ways of heating the vein. There’s microwaves or radio frequency which is the VNUS Closure. There’s laser which is very powerful electromagnetic energy. And there’s also steam. Steam is very popular in France: it was invented in France. I’ve been to Lille to see steam treatment and I’m not convinced that it’s the right way to go,it’s a little bit uncontrolled for my liking. And certainly NICE have put endovenous thermal treatment by VNUS Closure and Laser as number one. So the the ranking now is endovenous thermal treatment number 1, number 2 ultrasound guided foam sclerotherapy and coming in a poor third is surgical stripping. People say well which treatment is best? Well the best treatment number one is endovenous thermal treatment by laser or radio frequency VNUS Closure. There may be some reasons why foam sclerotherapy would be more suitable and that rather depends on the appearance of the veins on ultrasound. But these are things that you need to consider: obviously the cost; how quickly you want your veins to look better and feel better; time off work. I am going to have to take some of these out now I don’t think anybody wants to go into hospital. There are some people who do feel a little anxious about having their veins treated under a local anaesthetic. There are lots of advantages to having you rveins treated under local and certainly my preference is to treat veins under local anaesthetic – so much so in fact that I don’t perform any of my treatments now under a general anaesthesia.
Sclerotherapy may be more appropriate ifthe appearance is such that an endovenous thermal treatments not possible; but some people who are paying for themselves who can’t get treatment on the NHS may feel that for them it’s the most cost effective way of having their veins treated. But when you come for your consultation and we do your scan we’ll have an individualized program for you. Often people have more than one option and they have these various criteria to consider before making their own choice. Now this is the latest treatment it’s superglue it’s produced by an American company called Sapheon and it’s called Venaseal®. The vein is bonded in seconds. It doesn’t use heat energy; there’s only usually one local anaesthetic job necessary and there’s no need any stockings bandages or compression afterwards. So it’s a so-called tumescent–less that means it doesn’t require very much local anaesthetic; it’s non thermal there’s no heat energy involved; and it’s very quick and very minimal aftercare. People have no restrictions on them at all after this treatment. I’mgoing to show you a little short video of a Venaseal® procedure. There’s nothing gory here, so don’t need to look away. So this is the superglue itself; it comes in a little vial; it has a dispenser and a catheter that gets put into the vein. This is the glue being loaded onto the dispenser and that’s the catheter being inserted into the vein and a little ultrasound showing the catheter being pulled along the vein there’s the applicator and there’s a little scheme of the glue coming out of the vein. And this is our first case in the southwest where the gentleman was chatting to our nurse and he was very very comfortable. So one of the questions I get asked quite a lot is what happens to the glue, where does it go, will it move around my body or is it toxic? Well this is not just an ordinary superglue, it’s not the superglue you get from “B&Q” . It’s a medical superglue that’s been used in the body for 50years. It’s used to treat blood vessels in the brain, it’s used to treat damaged internal organs after road traffic accidents and it’s been shown over the50 years to be very safe. It doesn’t break down into anything toxic. It doesn’t cause cancer and the formulation for veins which Venaseal® is has been in development for five years. So it’s a particular formulation; it gets put in the vein that’s refluxing; it doesn’t move it stays where it’s put; it’s very quickly bonding so it closes the vein very very quickly and it won’t move around the body and go to the heart or go to the brain. So it’s very safe . It’s been available in the in Europe for about nearly three years now and we now have data coming out, albeit quite short-term, but the data we have shows that it’s as good as endothermal treatments and for people who don’t want a lot of local anaesthetic jabs who don’t want to wear stockings who want to be able to drive straight away it does have some potential advantages; and that’s superglue.
What about thread veins, how can we treat those? Well of course there’s camouflage. If you have a scan and it doesn’t show very much in the way of reflux and there’s no underlying problem you may be reassured you may not wish any particular treatment. In which case camouflage is an option. Having said that most people who get to the stage of seeing us and the clinic want something done about their thread veins. There are electrical treatments like electrolysis. They’re particularly good for thread veins on the face . There are treatments that involve putting a laser on the skin: that’s not the same as endovenous laser;but you can put a laser on the skin and you can treat those veins on the surface with laser. Again very good for the face and the chest but not so good for theleg. And then there are injection treatments again this is sclerotherapy using a different formulation for thread veins themselves which is the treatment that’s best for legs. This is how we treat thread veins on the legs. We use a very fine needle, we put a medical solution into the thread veins and they fill with sclerosant. They look as if they have disappeared because they become clear. Once again it works by removing the lining of the vein and causing the vein to shrink and collapse. This is a little video clip showing how the injection treatments are done. These are thread veins on the leg that have no reflux and I’m injecting a medical solution directly into the thread vein; and as you can see as the clear sclerosant displaces the blood they look as if they disappear. It works by removing the lining of the vein it starts a healing process. These thread veins are actually in the skin,they can’t be surgically removed or taken away. And a healing process is started and eventually those veins will disperse and become much less noticeable.
This is electrocoagulation, an electrical treatment for thread veins on the nose. We’re using a very fine needle and we’re applying a medical current to the veins to get them to collapse and disperse. And electrocoagulation is a very effective of dealing with thread veins on the face. I’m going to show you now just a very brief series of before photographs. On the left is the before in all cases and on the right is the after. This is a lady who had a nasty cluster of spider veins on her nose treated by her electrocoagulation. This is a lady who had quite severe varicose in her thigh and calf treated by VNUS Closure to the refluxing vein in her thigh and phlebectomy which is gently extracting the veins and that’s the result of treatment. In all cases the picture on the right is about six to eight weeks after treatment. And in fact this is the back of her legs; she had varicose veins quite severe in both legs. She had both legs treated at the same time under local anaesthetic as a walk-in walk-out procedure and that’s the result six weeks later. Men get varicose veins too – it’s not just ladies – and this gentleman had quite severe reflux in his thigh feeding into thighs and calf veins. He was treated by radiofrequency ablation. This is a view from the front these thigh veins and calf veins treated and six weeks later that’s the result.
Again this is another man just to show you that men do get veins as well. This was a member of airline crew, cabin crew who had a refluxing vein behind his knee causing quite a nasty little vulnerable bubble there on the back. He was concerned that it might get injured in the course of his work when he was up in a plane. There’s the back of his leg showing that nasty bubble and again that six weeks later. This lady has severe reflux in her thigh causing varicose veins and,I think you can see, she’s also got some varicose eczema. We treated the reflux and the varicose veins. The reflux is gone, the varicose veins have gone. The skin will improve, but in some cases there is damage beyond repair. And although the varicose eczema may well improve – in some cases it will go completely if it’s caught early and it hasn’t been present for a long time – ifit’s been present for a long time and it’s very severe it may not gocompletely and the skin as I say has been damaged beyond repair. Another series of photographs before and after showing the sorts of results. This was one of the most severe sets of veins we’ve treated recently. Not surprisingly,it’s in a man. When men do eventually come to see us their veins are usually very severe -and they tend to keep them covered under trousers -and when they do eventually come to see us they’re usually quite severe. He had both legs treated his right leg more severe than the left both legs treated at the sametime in one visit and that’s six weeks later. That’s the back of his legs there, showing the sorts of results we can achieve in six weeks. And some more before and after photographs. Thread veins. Now these take longer becausethey’re in the skin and because the healing process is slower you often need more than one injection treatment and the timescale is longer. So in this case this is six months. Good improvement, but not gone completely. They don’t always disperse completely.
